Frozen Embryo Transfer (FET)
Frozen Embryo Transfer (FET)
Frozen Embryo Transfer (FET) is a process in which an embryo that has been frozen during the previous IVF cycle is thawed and navigated into uterus of women. This prevents the need for further hormone stimulation and egg collection cycles.
Why it's done ?
- If the couple are not ready to be pregnant presently, they may undergo the embryo freezing technique.
- Sometimes, hormones are produced in very large numbers during ovarian stimulation because of the development of many follicles. In this condition, embryos are frozen to avoid a complication called Ovarian Hyper-Stimulation Syndrome (OHSS).
- If a large number of embryos are formed during the IVF cycle, usually one or two embryos are transfered and the rest of the embryos will be frozen to avoid multiple pregnancies and associated risks.
- Genetic disorders: If both couples have some genetic disease, inherited by the offspring, genetic screening is offered before implantation. Some cells are biopsied and genetic analysis is carried out. Healthy embryos are then transferred that are devoid of any illness.
- Preservation of fertility: When a female is treated for cancer, such as radiation or chemotherapy, that could harm her fertility, there is an option to freeze embryos. These can later be transferred following treatment with cancer.

How Do You Get Ready?
The first move is to seek the advice of a qualified reproductive endocrinologist. Both partners are likely to undergo multiple screenings before beginning an IVF cycle.
- For females: 1.Ovarian reserve testing determines the quality and quantity of eggs produced. In the early days of the menstrual cycle, blood levels of Follicle-stimulating hormone (FSH), Estradiol, and Anti Mullerian hormone are measured. Ultrasonography is often used to assess the amount of eggs in each ovary and how the ovary will respond to fertility drugs. 2.The lining of the uterus will be tested before the IVF procedure. A hysteroscopy is a procedure in which a small, flexible, lighted telescope (hysteroscope) is inserted into the uterus through the vagina and cervix.
- For males: sperm analysis is performed as part of the initial fertility assessment.
- For couples: HIV, Hepatitis B, and Hepatitis C are among the infectious diseases that can be detected by screening.
What can you expect ?
Since there are several steps to the operation, it will be explained to the patient:
1.Stimulation of the ovaries :
- injection FSH/HMG are given to stimulate the ovaries to produce several eggs instead of the single egg that forms normally each month. Since certain eggs will not get fertilize or grow normally after fertilization, multiple eggs are needed.
- Monitoring: The growth of follicles is monitored using vaginal ultrasound of the ovaries. Blood tests are also used to assess how well ovarian stimulation drugs are functioning — estrogen levels rise as follicles grow, while progesterone levels remain low until just after ovulation
- Oocyte Maturation Medication: Human chorionic gonadotropin (HCG) or other drugs are provided to help the eggs mature when the follicles are ready for egg retrieval, which usually takes eight to fourteen days.
2.Collection Of Eggs
- The egg retrieval procedure is usually scheduled 34 to 36 hours after the final injection and before ovulation. To render the treatment painless, it is performed under sedation.
- The most common form of retrieval is transvaginal ultrasound aspiration. A thin needle is inserted into an ultrasound guide to go through the vaginal canal and into the follicles to extract the eggs under ultrasound guidance.
- A needle attached to a suction system is used to separate the eggs from the follicles. In around 20 minutes, you can extract several eggs. The more the number of eggs retrieved, the better the chances of conceiving.
- The patient may experience cramping, fullness, or fullness after the egg retrieval procedure.
- Incubation is performed on mature eggs in a culture medium. Healthy fertile eggs will be combined with sperm in an effort to produce embryos.
3. Retrieval of sperm
If a partner’s sperm is used, he will have a semen sample the morning of ovum retrieval via masturbation. Other methods include testicular aspiration, which involves extracting sperm directly from the testicle with a needle or surgical procedure, which is often used, or donor sperm may be used.
4. Fertilization
Fertilization can be accomplished in one of two ways:
- Traditional insemination: In this process, mature eggs & healthy sperms are combined in a culture medium, where the sperm uses its natural motility to fertilize the egg.
- ICSI : single healthy sperm is inoculated directly into a mature egg in intracytoplasmic sperm injection (ICSI). When the quality or quantity of sperm is a concern or fertilization attempts during previous IVF cycles have failed, ICSI is often used
5. Freezing of embryos
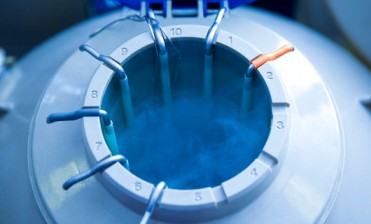
- Vitrification is the most common process used for embryo freezing. The water which is present inside the cell is replaced by cryoprotectants. It is followed by extremely rapid freezing, which prevents the formation of ice crystals within cells and thereby increases embryo survival while thawing. Embryos are then positioned in plastic straws and marked with the name and identification number of the patient. This process can be used to freeze embryos for many years if liquid nitrogen tanks are
Transfer of frozen embryo
- Uterine lining preparation: hormonal medicines are used for the development of uterine lining. The lining will be receptive to the embryo with Progesterone supplementation. The embryo transfer procedures are scheduled if the uterine lining is noted to have good blood flow and favorable thickness.
- A number of embryos to transfer : Typically, the number of embryos transferred is based on their age and egg number. Since the implantation rate for older women is lower, more embryos are generally transferred. For further use for several years, additional embryos may be frozen and saved.
- Thawing: Embryos are removed from the storage tank and then gradually warmed up to room temperature.
- The procedure for embryo transfer is usually painless, although the patient may experience mild cramps. Although the operation is usually painless, the patient may feel mild cramping. A catheter is a long, thin, flexible tube that is inserted into the vaginal canal, then passed through the cervix and into the uterus. The catheter’s end is attached to a syringe holding one or more embryos suspended in a small volume of fluid. The syringe’s contents are then injected into the uterus.
Post-Procedure Results
The patient will resume regular daily activities after the embryo transfer. However, since the ovaries may still be swollen, physical exercise may be uncomfortable and should be avoided. If you notice any of the following side effects, you can see a doctor right away: Pain in the abdomen, Heavily bleeding, and Urinary complaints
- A blood test (beta-hCG) is used to determine if the patient is pregnant 12 days to 2 weeks after embryo transfer.
- If the woman is pregnant and has a positive b-HCG test, the doctor will begin or refer her to prenatal care.
- If the woman is b-HCG negative, which means she is not pregnant, she should stop taking progesterone and expect to have her period within a week. If she still has some frozen embryos, she will be given frozen embryo transfer in subsequent cycles.
What Are the Consequences ?
- Ovarian Hyperstimulation Syndrome : which is a condition in which the ovaries are overstimulated
- Ovulation stimulation is a procedure in which women are given injectable hormone drugs to help them produce more eggs. The issue occurs when the body has an excess of hormones, which may lead to Ovarian Hyperstimulation Syndrome (OHSS). It’s a disease under which the ovaries swell up and cause excruciating pain. Abdominal pain, vomiting are associated problems.
- Multiple pregnancies: If more than one embryo transfer occurs, there’s a chance of multiple pregnancies, which may lead to early labor and low-birth-weight infants.
- When a fertilized egg implants outside of the uterus, normally in a fallopian tube, it is known as an ectopic pregnancy. The fertilized egg is unable to survive outside of the uterus, and will lead to termination of pregnancy.
- Birth defects: The mother’s age is the most important risk factor for the occurrence of birth defects.
Start your Parenthood Journey with Goodwill IVF
We have highly experienced team of fertility experts, including obstetricians and gynecologists, pediatricians, embryologists, andrologists, ultrasonologists, counselors, nurses, and other healthcare professionals always dedicated to help you.
Goodwill IVF
- A Unit of Neha Hospital, Changuvetty Kundu, Kottakkal, Kerala 676503
- Phone: +91 80897 13201
- Email: goodwillivf@gmail.com